Sean Overin
Sex, Pain, and the Conversations We Need to Have

How to approach sexual health in persistent pain care — without making it awkward
As clinicians, we often talk about stress, sleep, exercise, and nutrition — the usual pillars of well-being. But there’s one essential area of health that often stays off the table: sexual health and intimacy.
And yet, for many people living with chronic pain, sex is one of the first things affected — and often the last thing addressed.
Sometimes it’s not even voiced aloud. Maybe it shows up as “wanting to feel like myself again,” or “getting back to my relationship,” or “feeling confident in my body.” These are deeper motivations — unsaid personal goals — that may go unspoken unless we create the space.
So we have to ask ourselves:
👉 Are we really getting to the heart of what matters to them?
👉 Are we inviting the kind of honesty that makes healing possible?
What Recent Research Says...
In a recent study published by Flegge et al., 2023 surveyed 247 adults living with chronic pain about their sexual functioning. Over 70% of those who were sexually active reported challenges in at least one domain.
Here’s the breakdown:
For participants who identified as women, the most common issues were low sexual interest, dissatisfaction, and high vaginal discomfort — and these weren’t just random or isolated experiences. They were closely tied to the intensity of pain they were living with, along with symptoms of depression and anxiety.
👉 In other words: the more pain and emotional distress someone was experiencing, the more likely it was affecting their sexual well-being — physically and emotionally. It’s all connected.
For participants who identified as men, the picture looked different. Sexual difficulties like low desire and dissatisfaction were common, but surprisingly, they weren’t significantly linked to pain or mood symptoms in this study.
👉 That raises important questions:
1. Are men less likely to report emotional or physical pain related to sex?
2. Are they feeling it but not naming it?
3. Could stigma or internalized beliefs about masculinity be getting in the way of disclosure?
Either way, it’s a clear sign: we want to create safer, more open spaces for these conversations — for everyone.
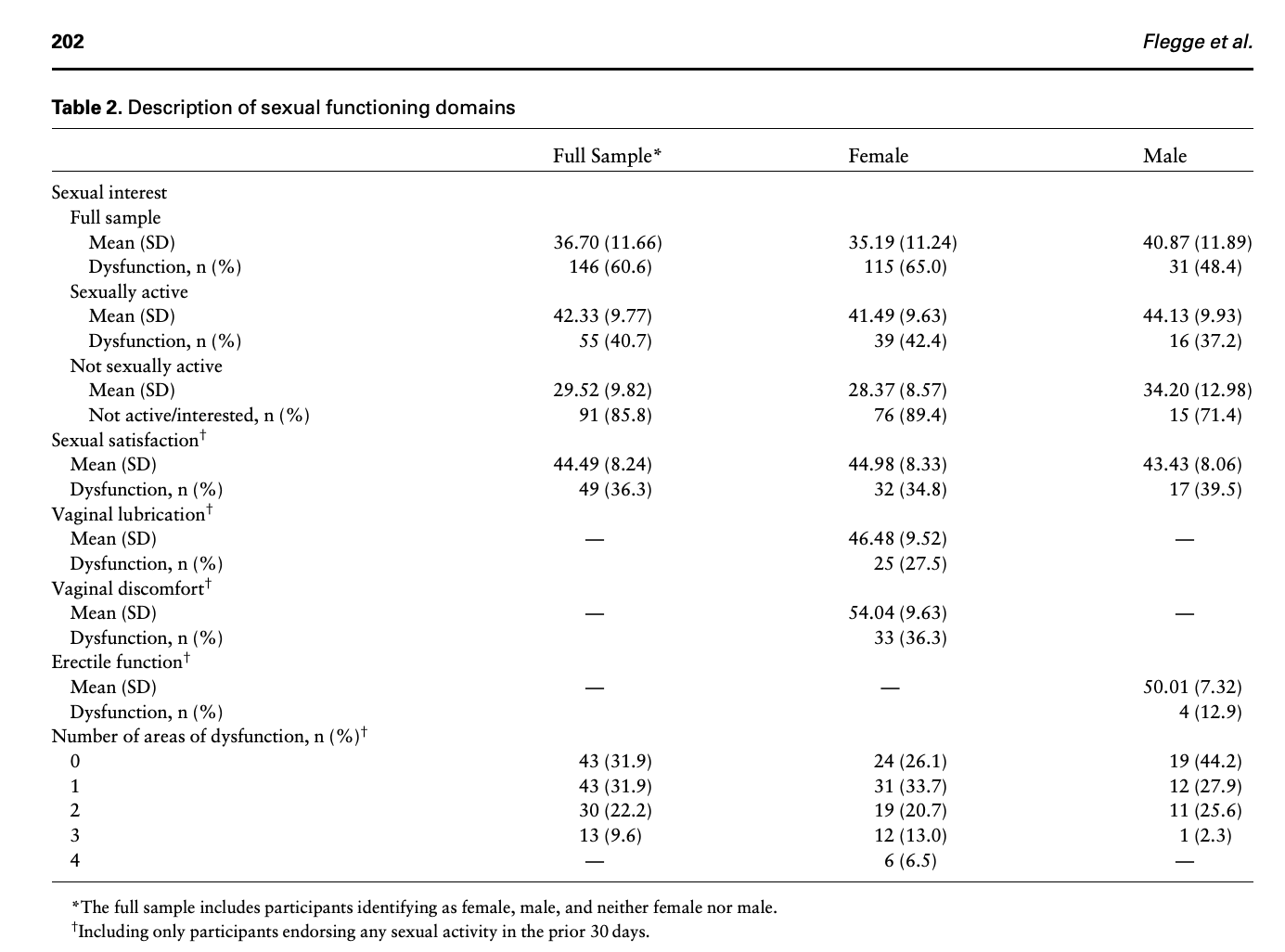
Table from Flegge et al. 2023.

Rethinking the Conversation
One reason this topic stays hidden? We don’t always know how to bring it up — or we worry about making the client uncomfortable. But sometimes it’s all about the how.
Instead of jumping straight into:
❌ “Are you sexually active?”
❌ “Are you sexually active?”
Try:
✅ “Has your pain affected your sense of closeness or connection in relationships?”
✅ “Sometimes pain impacts intimacy — has that been part of your experience?”
✅ “Has your pain affected your sense of closeness or connection in relationships?”
✅ “Sometimes pain impacts intimacy — has that been part of your experience?”
These questions feel safer, more open, and more inclusive — and they create space for a meaningful conversation that many clients are waiting for someone to initiate. There are many different ways to bring up the topic, but if your looking to get started, those are a few.
A Book That's Worth a Read: Come As You Are
If you haven’t read Emily Nagoski’s Come As You Are go check it out.
This book should be on every clinician’s shelf — especially those working in persistent pain, pelvic health, or mental health. Nagoski breaks down how desire, arousal, and pleasure are shaped by context, stress, trauma, and culture — not just hormones or mechanics.
One of her core models is the dual-control model of arousal: the brain has both an accelerator and a brake. Pain, fear, stress, and shame can slam on the brakes — even when the desire to connect is there.
💡 “Lack of interest isn’t a dysfunction — it’s information. It means the brakes are on. And that’s your body protecting you.”
— Emily Nagoski
When we understand this, we can stop trying to “fix” low libido — and instead focus on creating safety, trust, and the right context for connection.
The keys to a happier, healthier sex life. Worth considering this when working with patient's with persistent pain.
Resources ...
A Resource to Share with Clients
If you’re looking for something to offer clients directly, check out this helpful, inclusive resource from Pain BC:
It’s practical, compassionate, and written in clear, relatable language that helps normalize the impact of pain on intimacy and relationships.
💡 Clinician tip: Scroll to the bottom — it includes more resources for clients, partners, and care providers.
Final thoughts ...
Sexual health is health. And when we ignore it in the context of chronic pain, we miss a huge part of what makes life meaningful. Clients may not always have the language to bring it up, or the safety to speak about it — but we can create that space.
Because what happens in the bedroom often stays unspoken in the clinic. And it’s time that changed.
Want to go deeper?
Join the conversation with our AMP community — or reach out for handouts, scripts, or training resources for your team.
Let’s keep learning, keep listening, and keep making healthcare the way it should be.
Supporting Clinical Resources
Get the clinical knowledge and practical tools you need to confidently assess, treat, and support menopausal clients more effectively.
The Clinician’s Guide to Exercise and Pain
Evidence-based tools and strategies to confidently support safe, effective movement in people in pain.
Build stronger, more meaningful therapeutic relationships with insights from top clinical experts.
Sean Overin, MPT, tDPT Registered Physiotherapist
Subscribe to our newsletter
Every Friday we cover must read studies, how they fit in practice, give it real world context, provide top resources and one sticky idea.
Thank you!
You have successfully joined our Friday 5 Newsletter subscriber list.
