If you ask most rehab professionals what their patients want, the answer seems obvious:
to get 'better.' That was my assumption early in my career. I figured my job was to:
- Ask the right questions
- Perform the best objective tests
- Create a solid treatment plan
- Prescribe the right exercises
- Maybe do some manual therapy
Do all that, and patients should be happy, right? Well… not exactly.
Over time, I started noticing a disconnect. Some patients didn’t follow the plan but kept coming back and were satisfied with their care. Others had great outcomes but didn’t seem that impressed.
Something wasn’t adding up. So, I started looking into the research. What do patients actually want from us? Turns out, a lot of what I assumed wasn’t quite right.
Here’s what I found, and more importantly, how you can use this information to level up your practice starting tomorrow.
Physiotherapist Louis Gifford, a highly influential physiotherapist who helped advance clinical reasoning and integrate the biopsychosocial nature of pain into practice, was one of the first to understand what patients really want from their care. He proposed
four key questions that he thought every patient is trying to answer:
- What’s wrong with me? (Diagnosis)
- How long will it take to get better? (Prognosis)
- What can I do to help myself? (Self-management)
- What can you do to help me? (Treatment expectations)
Recent
research supports these questions, showing that they’re the foundation, not only thing, that patient's want from a physiotherapist. If we fail to answer them clearly, patients may leave feeling uncertain, even if our treatments are clinically sound.

Strategy #1: Build These Four Questions Into Your Sessions
- Start by addressing uncertainty. Even if you don’t have a definitive answer, say, “Based on what you A, B, and C from your history and D, E and F in the objective exam, this is what I think is going on…”
- Give a realistic prognosis. Instead of vague timelines, frame it like: “Most people with this condition see improvement in 6-8 weeks, but we’ll track your progress and adjust as needed.”
- Clarify the patient’s role. Patients want to know exactly what they need to do. Be specific: “Your key exercises are A and B. I will send them to you. Do them X times per week. If you miss a day, no big deal—just keep going.”
- Explain your role in their recovery. Set expectations: “I’ll guide you through this process, track your progress, and adjust things as needed.”
Of course, every patient will a diverse set of expectations and needs so I think its unreasonable to expect these questions will answer everything that is relevant. But it should serve as a great starting point.
A systematic review by
Hush et al. (2011) analyzed patient satisfaction in musculoskeletal rehab. One surprising finding? Satisfaction was more influenced by the
quality of the clinician-patient interaction than by clinical outcomes.
In other words, even if someone doesn’t fully recover, they can still be highly satisfied if they feel heard, respected, and engaged in their care.
Strategy #2: Improve the Experience of Care
- Be warm and present. Small things—eye contact, a friendly greeting, remembering details about their life—make a huge difference.
- Summarize and reflect. Before jumping into solutions, say: “So what I’m hearing is…” and summarize their concerns.
- Patients feel heard when they know you understand them. Validate and normalize. A simple, “That makes total sense—dealing with pain is exhausting” goes a long way.
- Involve them in decisions. Even small choices, like whether they want to focus on movement drills or pain management first, can increase buy-in.

Bernhardsson et al. 2017 study found that 96% of patients want clear guidance on what to do and what to avoid. But many patients report
getting conflicting advice from Dr. Google, well-meaning friends, and even different healthcare providers. In my practice I have seen a trend of patient's completely avoiding the internet and showing up on my doorstep to just cut-through all the noise and get to a personalized understanding and plan as to what is happening.
Strategy #3: Cut Through the Noise
- Provide a simple, personalized, and memorable explanation. Avoid jargon. Instead of “you have rotator cuff tendinopathy”, try: “You have rotator cuff tendinopathy, which means your shoulder tendons are a bit cranky because of X, Y, and Z from what I heard today."
- Give clear ‘dos and don’ts’ but with flexibility. Instead of rigid rules, say: “These movements are usually helpful, but let’s see what works best for you.”
- Address misinformation head-on. If a patient says, “I read online that I should never squat past 90 degrees”, respond with: “That’s a common belief, but research actually shows…”

From Subialka, Hush and Bernhardsson, all found that patients expect a structured plan for their recovery—not just a one-off visit with a sheet of exercises.
Strategy #4: Map Out the Road Ahead
- Give a timeline. “In the next six weeks, we’ll focus on A and B. After that, we’ll shift to C.” Right this out and ensure they leave with this! People are well-intentioned however they forget most of what is said.
- Reassess frequently. Patients appreciate knowing how they’re progressing. Try: “Last week, you could only do X reps, now you’re at Y. That’s progress.”
- Book follow-ups strategically. Instead of “Come back if you need me”, say: “Let’s check in once per week for the next 4-weeks to tweak things and make sure what we're doing is actually working."
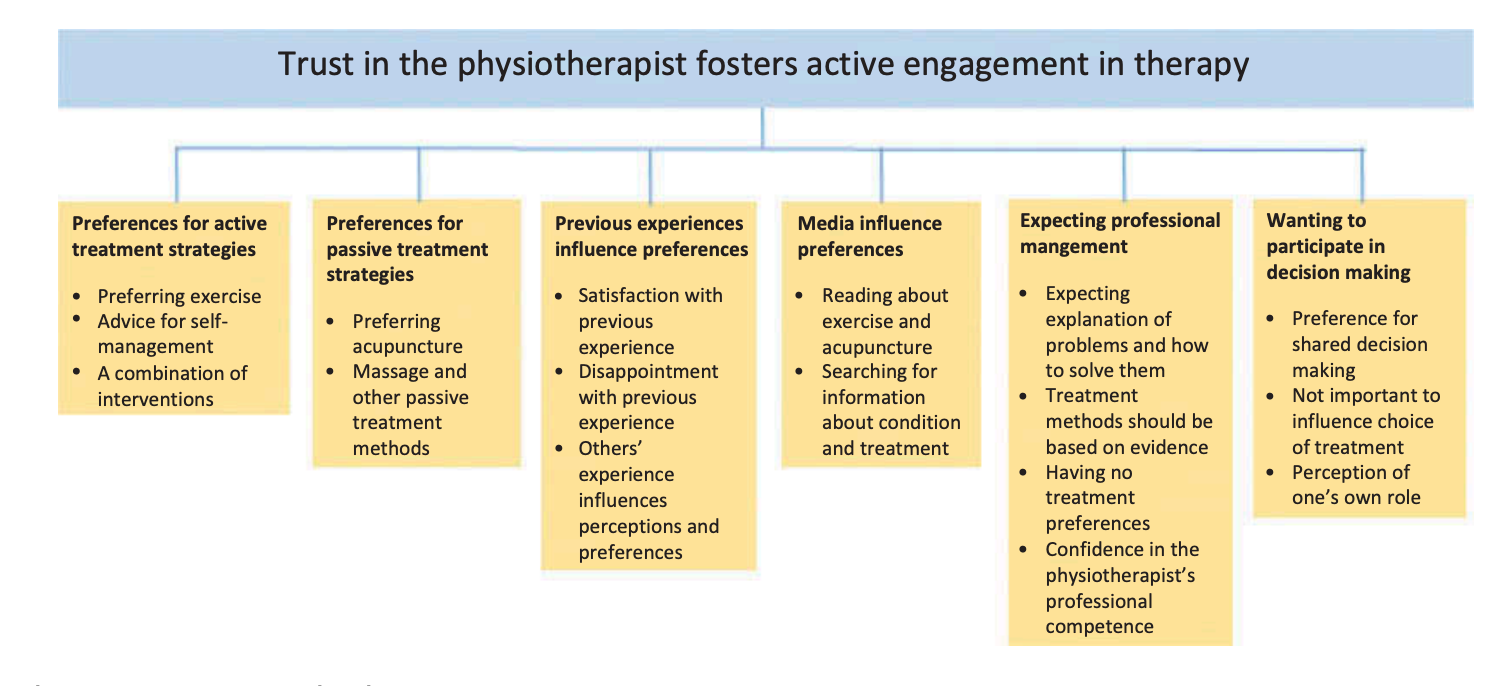
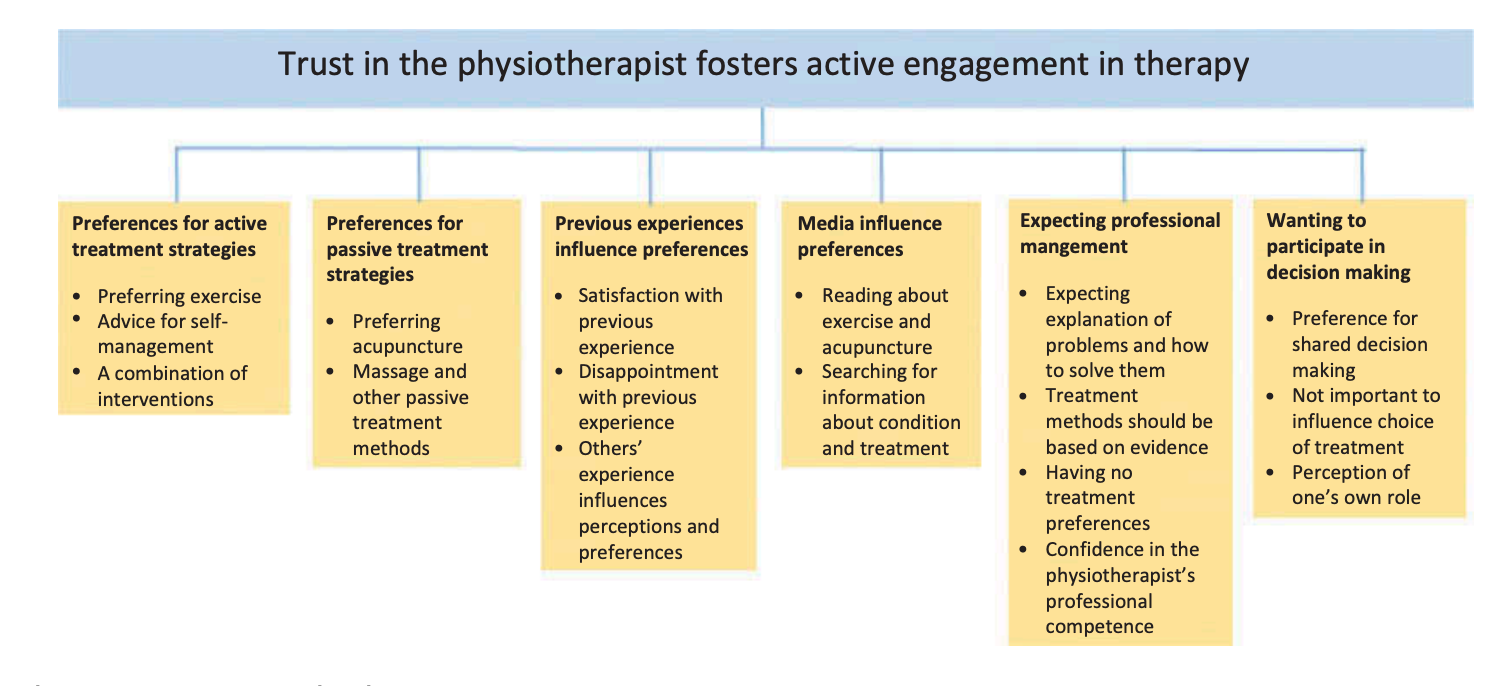
Figure 1: From Bernhardsson et al. 2017.
6 themes that emerged from this qualitative study listed above.
Bernhardsson (2017) found that about 70% of patients prefer a collaborative model, where decisions are shared between patient and clinician. This really fosters trust-building and the formation of a partnership. But a small percentage want to be fully led, while others prefer to take the lead themselves.
Strategy #5: Adapt to Their Decision-Making Style
- For patients who want to be led: Be confident but open. “Based on the what I am seeing and hearing, I recommend X, Y and Z. How does that sound to you?”
- For patients who want more control: Engage them in the process. “There are a few good options here. What do you think fits your lifestyle best?”
- For patients unsure about their role: Use gentle prompts: “Some people like to be hands-on with their rehab, others prefer more guidance—what feels right for you?”
Patients want more than just symptom relief—they want clarity, structure, and a sense of control. Here are five key ways you can improve their experience:
- Answer the Four Golden Questions. Make sure every patient knows their diagnosis, prognosis, role, and treatment plan.
- Improve the experience of care. Listening, warmth, and validation matter just as much as clinical skills.
- Be an educator. Cut through misinformation and give patients clear, actionable knowledge.
- Create a structured plan. Set expectations, track progress, and book follow-ups with purpose.
- Adapt your style. Some patients want to be led, others want to collaborate—adjust accordingly.
At the end of the day, we’re not just treating injuries—we’re treating people.
So let’s make sure they leave our care feeling empowered, engaged, and seen.
If you want to learn more about patient-centred care check out our course!
Sean Overin, MPT, tDPT Registered Physiotherapist