Nov 12 • Sean Overin
Behavioral Science in Clinical Practice: Small Shifts, Big Gains

Thanks for tuning in! I wanted to share a recent case with a patient of mine, “James,” who’s been dealing with chronic back pain for years. It’s a powerful example of how simple behavioral change techniques—like active listening and self-monitoring—can make a huge difference in patient care. In my physio training, we didn’t really cover the psychology behind helping people make these kinds of changes, yet it’s a huge part of what our patients often need. Chronic conditions like back pain aren’t just physical; they impact every part of a person’s life.
With James, I found that slowing down, listening deeply, and giving him tools to monitor his progress turned out to be more impactful than any exercise I could prescribe. I hope this example gives you some ideas for your own practice. These techniques aren’t complex, but the impact can be huge.
Meeting James: Understanding His Struggles
James is a 55-year-old who’s been struggling with chronic low back pain for years. He’s tried all sorts of treatments—massage therapy, physical therapy, seen specialists, tried various medications, had lots of scans—you name it. But he came to me frustrated and, honestly, pretty defeated, saying things like, “Nothing works,” and “It feels like I’m going backward.” His back pain was affecting his mood, limiting his activities, and keeping him from things he enjoyed. On top of that, James was avoiding movement because he believed it would worsen his pain and lead to more damage, which only increased his sense of being trapped.

The Power of Listening
It’s easy to jump straight into solutions with patients, but as many of you know, sometimes the best thing we can do is just listen. So, with James, I didn’t jump into a plan or offer advice right away. I just listened. I didn’t interrupt or steer the conversation; I let him share what was on his mind. He opened up about feeling like a failure each time the pain returned and how the ups and downs made him feel stuck. By truly listening—reflecting his words back and asking open-ended questions—I learned so much about his beliefs, his fears, and the mental hurdles he was facing. This was valuable information that would later shape our conversations, advice, and his plan.
Active listening isn’t just about hearing words; it’s about understanding what the patient is really going through. With James, we quickly realized he didn’t just want pain relief; he wanted to feel empowered again. Once he felt understood, our session took on new energy. He started expressing his own ideas about what he was willing to try, which were incredibly helpful in shaping our path forward. This approach helped us move away from a top-down, “do this” approach and into a more collaborative, shared decision-making process.
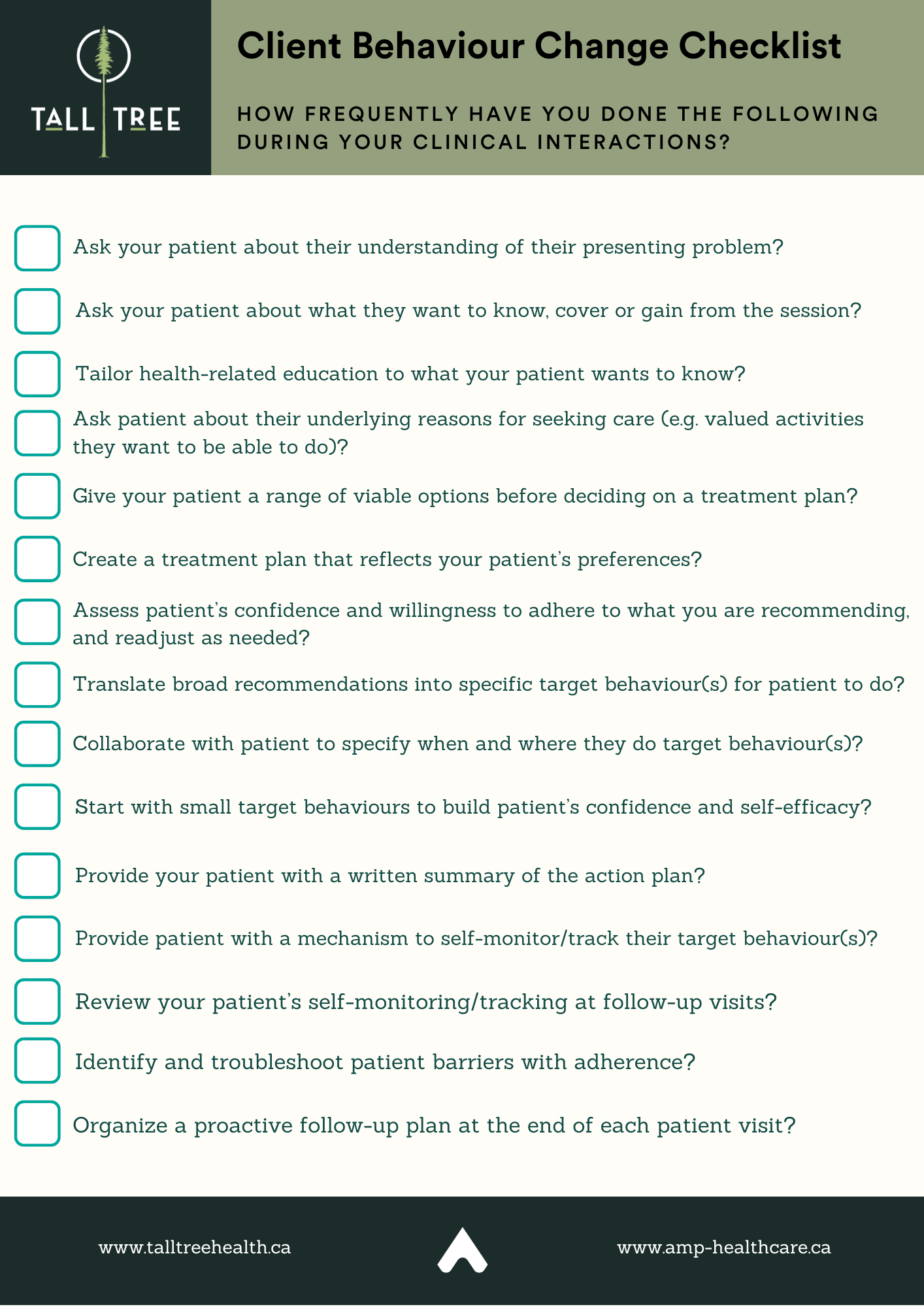
This checklist is from our intro and masterclass behaviour change courses ...
notice the 3rd question from the bottom ;)
Adding Self-Monitoring to the Mix
After our initial breakthrough, I introduced self-monitoring as a way for James to feel more in control and to highlight the wins along the way. He was open to trying it, so we started small—I suggested he track his daily walks by marking a check on a calendar near his front door. I highlighted that the goal wasn’t instant change or perfection, but to help him see patterns, track wins, and feel in charge of his health. He suggested we start with four 15-minute walks per week, which felt doable to him.
The results surprised both of us. By self-monitoring, James noticed that his fear of movement was often worse than the pain itself. He saw that a gentle walk might bring some initial discomfort but didn’t worsen his pain long-term. These “aha” moments helped him start reframing his relationship with movement. He felt encouraged—and even a bit proud—as he tracked improvements in how he felt about his body. Over the month, he started seeing all the checkmarks sprinkled across his calendar, but importantly, he naturally started walking more at greater intensities, noticed better sleep, fewer flare-ups, and even more enjoyment in daily activities. Win, win, win!

The Outcome: Small Steps, Big Changes
Through active listening and self-monitoring, James and I turned his approach to pain management around. We didn't do anything fancy or try to explain his lack of progress by using complex models. We used very simple tools grounded in evidence. And true, he didn’t find an instant cure and for many problems of life their isn't one, but his whole outlook shifted. Our conversations became more about problem-solving together and less about me “fixing” his pain. He started setting his own goals, which gave him a renewed sense of control. Our sessions became about building resilience and self-efficacy rather than eliminating symptoms. If there is one thing we have learned from clinical practice and the literature about people who have good self-efficacy, it is that they do ... well, you know how they do right? They do much better than those who don't have it in the short and longer term.
This experience with "James" has reminded me that sometimes the simplest tools can lead to the most meaningful changes. Small steps can lead to big shifts, it's a 1+1 = 10, and it’s incredibly rewarding to see patients take ownership of their journey—this is the kind of change I am sure we would all love to see in all our patients.
More Learning
So, I hope this case was intriguing and insightful. Treatment does not need to be complex to be effective. In this case, it was just about taking the time to deeply listen and giving patients a way to track their own progress, step by step. This doesn't work for everyone, but for some it can do wonders. Thanks for reading, and cheers to creating more meaningful change in our patients’ lives!
If this approach to patient care resonates with you, I’d love to invite you to explore two courses we’re offering to dive deeper into these essential skills:
1. Behaviour Change in Practice: – This shorter course provides a foundation in key behavioural science techniques. It’s perfect if you’re looking to add practical tools to your sessions quickly and effectively.
2. Changing Behaviour: A Masterclass for Health Professionals – For a more in-depth journey, our full course covers a comprehensive set of strategies to integrate behaviour change into all areas of your practice. This masterclass will equip you with advanced tools to transform how you approach patient care, fostering lasting change and better outcomes.
Both courses are designed to make behaviour change accessible and actionable for any healthcare professional or whether you’re new to the topic or looking to refine your skills. I hope you’ll join us and see firsthand the impact these techniques can have on your practice!
Sean Overin, MPT, DPT Physiotherapist
Subscribe to our newsletter
Every Friday we cover must read studies, how they fit in practice, give it real world context, provide top resources and one sticky idea.
Thank you!
You have successfully joined our Friday 5 Newsletter subscriber list.
