In the hustle and bustle of clinical practice, some essential tools can slip through the cracks. Treatment planning is one of those tools—often recognized as important but underutilized. Let’s unpack what treatment planning is, why it’s vital for patients and clinicians alike, and explore the common barriers that prevent it from happening.
At its core, a treatment plan is a collaborative roadmap between clinician and patient, designed to address health concerns and achieve specific goals. It typically includes:
- A clear assessment of the patient’s current health status.
- Shared, achievable goals based on the patient’s needs and preferences.
- Tailored interventions, such as therapies, lifestyle changes, or medications.
- A timeline for implementation, prognosis, and follow-ups.
Treatment planning isn’t just about logistics—it’s a conversation that fosters trust, clarity, and collaboration. Patients value treatment plans because they reduce uncertainty, empower them to take ownership of their care, and provide a sense of direction. Clinicians benefit too, as these plans enhance adherence, improve outcomes, and build stronger therapeutic alliances.
Patients want to know what’s next. Having a general roadmap reduces anxiety, builds confidence, and encourages active participation in their recovery. For clinicians, treatment planning offers structure and helps ensure that care is evidence-based, measurable, and goal-driven. Comprehensive treatment plans also allow for flexibility and adaptability, making it easier to adjust interventions as the patient’s needs evolve.
But despite their clear benefits, treatment planning doesn’t always happen. Why?
Patient Funding or Resources
Clinicians may feel a mental or emotional block when creating plans, worried about presenting options that could place financial strain on the patient. This anxiety can lead to hesitation or overly simplified plans that don't fully address the patient's needs.
In busy clinical environments, time is often the biggest obstacle. The focus is often on immediate interventions and managing patient expectations, leaving little room for a structured treatment planning process. While this is understandable, skipping this step can leave patients feeling uncertain and less engaged in their care.
Intolerance to Uncertainty
Treatment planning requires clinicians to grapple with the inherent uncertainties of healthcare—diagnoses that aren’t black and white, prognoses that are variable, and treatment pathways that may not be linear. The process involves synthesizing complex clinical information, setting measurable goals, creating timelines, and clearly documenting these for both the patient and clinical records. For some, this can feel daunting or overwhelming, leading to avoidance or minimal engagement.
Fear of Sounding Like a Salesperson
Discussing long-term plans or additional treatments can feel awkward. Many clinicians worry that these conversations may come across as sales-driven rather than patient-centered. This fear can lead to overly cautious or vague communication, which undermines the benefits of a clear and empowering treatment plan.
While treatment planning is introduced in entry-level training programs, the practical application often lacks depth. Without a clear understanding of expected recovery timelines or prognosis, some clinicians may feel ill-equipped to develop and communicate an effective plan. Additionally, many clinicians lack a system or habit of routinely incorporating treatment planning into their practice. Without this structure, treatment planning can feel like an extra step rather than a seamless part of patient care. Developing a consistent approach to treatment planning—one that becomes second nature—can bridge this gap and ensure it’s an integral part of every clinical interaction.
Recognizing these barriers is the first step in overcoming them. Here are a few strategies to make treatment planning a more consistent and valuable part of your practice:
- Prioritize Collaboration: Engage your patients in the process. Ask about their goals, preferences, financial constraints and concerns to co-create a plan that resonates with them. Do this throughout the session and summarize it all at the end.
- Start Small: Treatment planning doesn’t need to be big and overwhelming. Focus on setting one or two clear goals with a general timeline and build from there. Perhaps printing off a few treatment plan cards would be a place to start and writing out the clinical impression for each new assessment.
- Reframe the Conversation: Instead of worrying about sounding salesy, view your role as a guide offering tailored recommendations. Patients value clear direction when it comes from a place of care and expertise. Your supporting not selling.
- Invest in Training: If you’re unsure about timelines, prognosis, or how to structure plans, seek out professional development opportunities. The more confident you feel, the easier treatment planning will become.
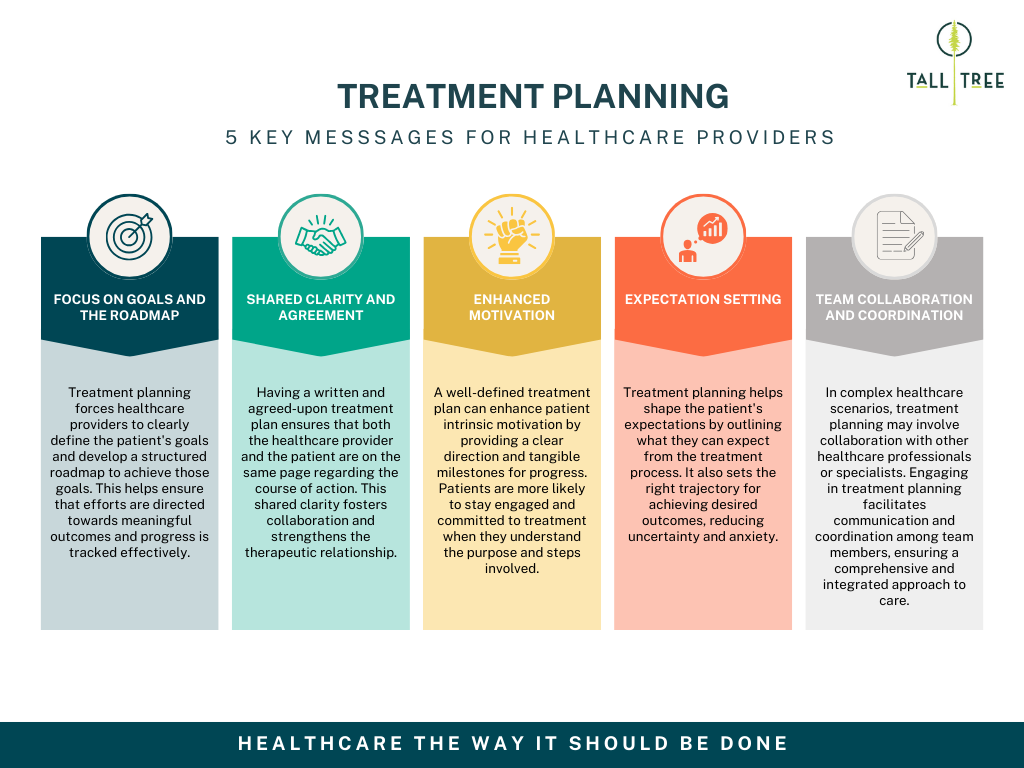
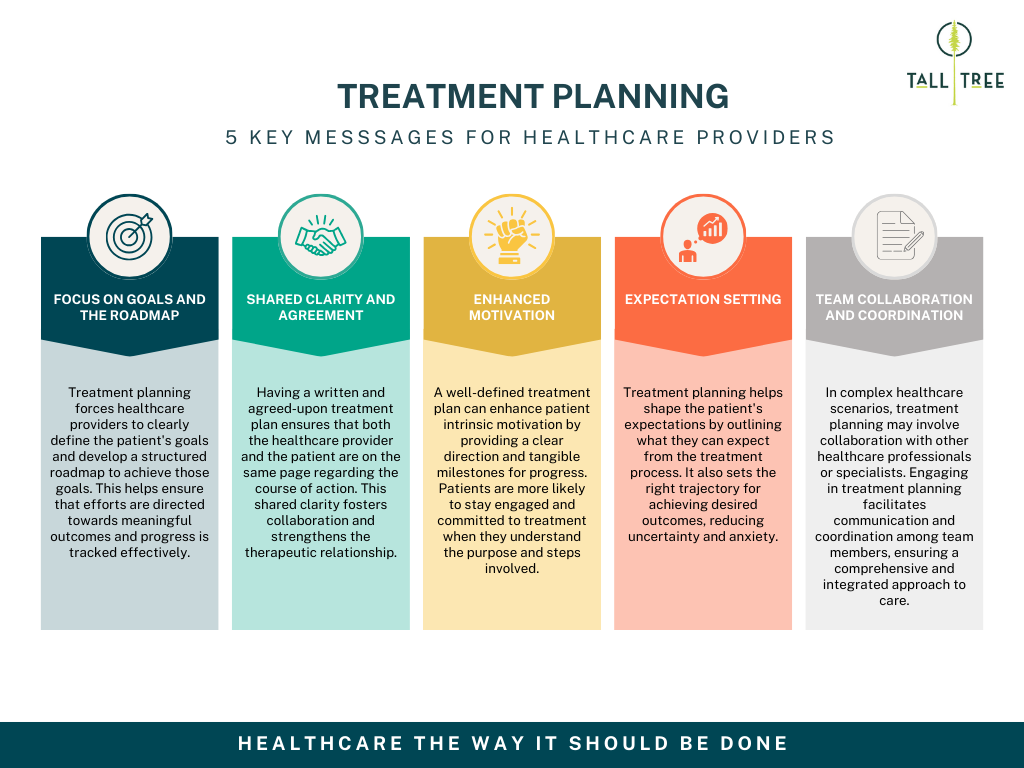
Summary slide from our Treatment Planning Course
Master Treatment Planning with Our Short Course
If this blog resonates with you, you’re not alone. Many clinicians find treatment planning challenging, but it’s also one of the most impactful ways to enhance patient care and outcomes. That’s why we created a short course on
Treatment Planning, designed to provide you with actionable strategies and practical tools to integrate into your practice immediately.
In the course, you’ll:
- Understand the key components of an effective treatment plan.
- Learn how to collaborate with patients to create shared goals and reduce uncertainty.
- Discover simple ways to incorporate treatment planning into your workflow without adding stress.
- Gain confidence in addressing prognosis, timelines, and interventions.
Thanks for reading! Stay impactful! And perhaps see you on the course!
Sean Overin, MPT, DPT Physiotherapist