Putting Physiotherapy First: What can we do for lateral epicondylalgia?
Write your awesome label here.
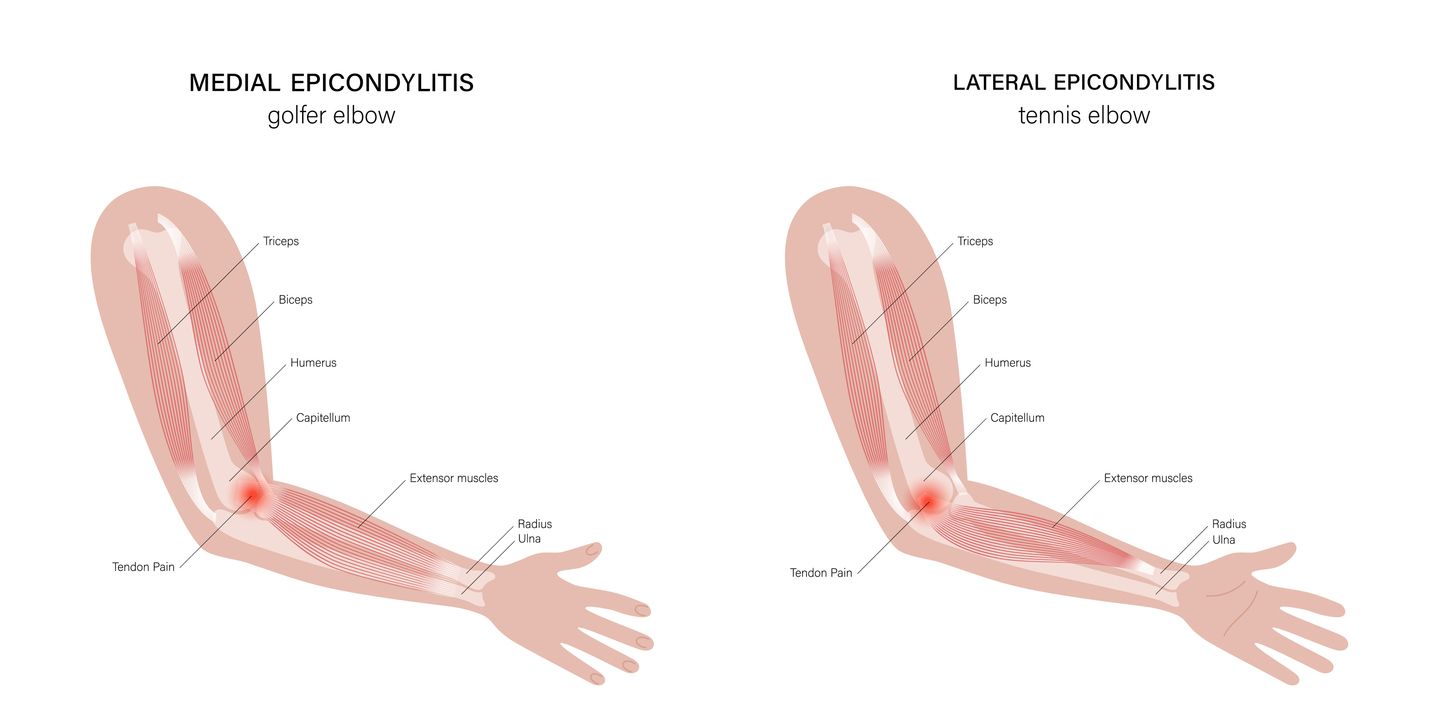
Lateral Epicondylalgia (LE) is a common condition typically affecting middle aged adults. Although once believed to be an overuse injury with an inflammatory component, more recent evidence suggests a continuum of changes in the local tissue termed angiofibroblastic hyperplasia, which suggests the following: 1) increased cell numbers and ground substance; 2) vascular hyperplasia or neovascularisation; 3) increased concentration of neurochemicals and 4) disorganised and immature collagen1. Furthermore, LE changes the motor system, decreasing pain-free grip (PFG) and alters the pain system resulting in neurogenic inflammation and/or central sensitization. This new knowledge prompted the renaming of the condition from lateral epicondylitis to lateral epicondylalgia.
Cortisone injections (CSI) were once a commonly used treatment for LE, but two recent clinical trials suggest that physical therapy may provide superior outcomes for the condition. In 2006, Bisset et al. compared three groups: 1) CSI, 2) physiotherapy based treatment that included mobilizations with movement (MWM) and exercise and 3) a wait and see group2. Although those patients treated with CSI demonstrated a significant improvement at six and 12-week follow-up, they demonstrated the worst outcomes at one year. The physiotherapy group demonstrated superior outcomes than the wait and see group at six and 12-weeks, but the differences were no longer significant at one year follow-up. A closer look at the data suggests that most patients in both the physiotherapy and wait and see group had fully recovered at one year, suggesting that LE may be a self-limiting condition but that physiotherapy treatment can speed recovery.
A more recent trial appears to support these findings. Coombes and colleagues produced a high quality, four arm trial comparing physiotherapy with CSI, physiotherapy with placebo injection, CSI alone, and placebo CSI3. Similar to the Bisset trial, the physiotherapy treatment included the use of a MWM technique (A lateral glide at the elbow joint) along with an exercise program. Again, a significant improvement was noted in those patients receiving cortisone over the first few weeks, but at one year follow-up 55% of CSI patients had a recurrence compared with only 5% of those receiving physiotherapy. At one year, all groups demonstrated a greater than 80% recovery rate with the physiotherapy group demonstrating a 100% rate of recovery. Noteworthy, at four weeks, 39% of the physiotherapy group with placebo injection demonstrated recovery compared to 0% of the placebo injection group, again suggesting that physiotherapy has a role in speeding recovery. There is also a developing body of literature to support the use of manual therapy to the cervicothoracic region in conjunction with standard treatment for LE. Cleland et al. found that those patients treated for LE with both local and cervical spine treatment demonstrated faster recovery 4. In a pilot randomized trial, Cleland demonstrated improved outcomes with those patients receiving manual therapy to the cervical region along with concurrent elbow treatment when compared to a group receiving only elbow treatment5. Fernández-Carnero et al. demonstrated that a single cervical manipulation caused an immediate decrease in pain pressure thresholds (PPT) and increase in pain free grip (PFG) in ten patients presenting with LE6. Vicenzino conducted a randomized controlled trial performing a lateral cervical glide combined with a neurodynamic technique compared to a sham technique and no intervention7. He found a significant immediate improvement in PPT, PFG and retesting of neurodynamics in only the lateral glide group. It should be noted that while many of the trials looking at the influence of cervical-based treatment are small or have short follow-up durations, the findings are promising.
A more recent trial appears to support these findings. Coombes and colleagues produced a high quality, four arm trial comparing physiotherapy with CSI, physiotherapy with placebo injection, CSI alone, and placebo CSI3. Similar to the Bisset trial, the physiotherapy treatment included the use of a MWM technique (A lateral glide at the elbow joint) along with an exercise program. Again, a significant improvement was noted in those patients receiving cortisone over the first few weeks, but at one year follow-up 55% of CSI patients had a recurrence compared with only 5% of those receiving physiotherapy. At one year, all groups demonstrated a greater than 80% recovery rate with the physiotherapy group demonstrating a 100% rate of recovery. Noteworthy, at four weeks, 39% of the physiotherapy group with placebo injection demonstrated recovery compared to 0% of the placebo injection group, again suggesting that physiotherapy has a role in speeding recovery. There is also a developing body of literature to support the use of manual therapy to the cervicothoracic region in conjunction with standard treatment for LE. Cleland et al. found that those patients treated for LE with both local and cervical spine treatment demonstrated faster recovery 4. In a pilot randomized trial, Cleland demonstrated improved outcomes with those patients receiving manual therapy to the cervical region along with concurrent elbow treatment when compared to a group receiving only elbow treatment5. Fernández-Carnero et al. demonstrated that a single cervical manipulation caused an immediate decrease in pain pressure thresholds (PPT) and increase in pain free grip (PFG) in ten patients presenting with LE6. Vicenzino conducted a randomized controlled trial performing a lateral cervical glide combined with a neurodynamic technique compared to a sham technique and no intervention7. He found a significant immediate improvement in PPT, PFG and retesting of neurodynamics in only the lateral glide group. It should be noted that while many of the trials looking at the influence of cervical-based treatment are small or have short follow-up durations, the findings are promising.

