Write your awesome label here.
As the early goldilocks exercises prove to be well tolerated, think about including some ‘core’ exercises, as well as isotonic and eventually eccentric hamstring exercises. Again use irritability to gauge when to progress. Spend time on other impairments also. Screen mobility, strength, movement, and the regional joints at the initial and over the course of early rehab.
Don’t forget to include running progressed to sprinting as part of a return to sport for this population. Sprinting is often the mechanism of injury, and that makes it an important activity to expose your patient to in a progressive and controlled context. Consider the benefits from both a physical and a psychological perspective.
Now, is there anything else that we can do to help reduce pain and increase function? Alas, there is a paucity of evidence for the role of manual therapy to treat HSI (2). Regardless, there’s a decent argument to screen for impairments at the lumbo-pelvic region, hip, knee, foot, and ankle. As always, find your asterisk signs, and try to change these with various interventions such as manual therapy, needling, tissue distraction, ISTM, foam rolling etc. Even if these changes are short-lasting and work on the nervous system, we can modulate the signal going in (i.e. the afferents) and influence the output (i.e. pain). This demonstrates to our patient that their symptoms are malleable and can be reduced, which can help shape a positive outlook on their prognosis. Manual therapists sometimes call these changes the “window of opportunity.” But before “opening the window” there are some things to think about.
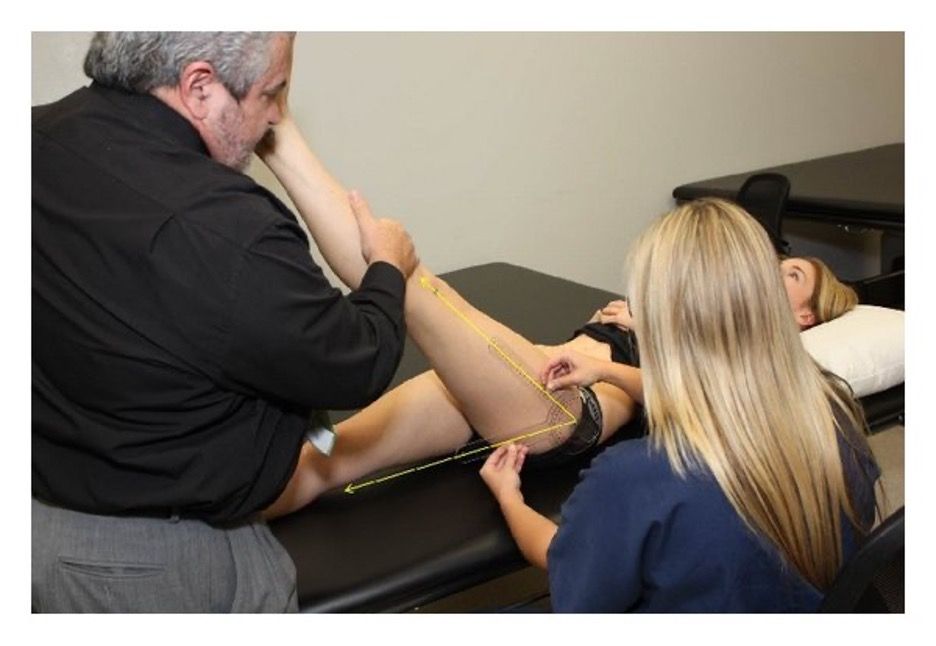
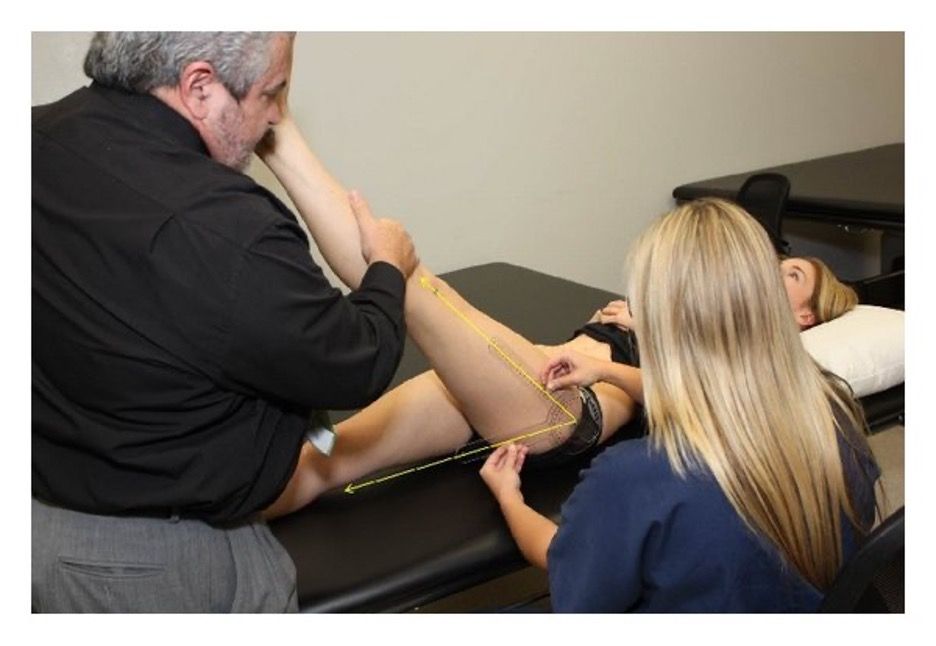
Adverse NeuroDynamics (AND) are another avenue of exploration. AND are a recurring theme within the literature on HSI, but the relationship is not robust. A few studies have examined to see if neural tension predicts HSI, but neither the Straight Leg Raise (SLR) or the Slump test were able to do so (2,3). Despite the lack of predictive power, neurodynamic treatment is often advocated for in the treatment of HSI (4).
One recent study showed that SLR range of motion was immediately improved by a slider technique, better than static stretching or control group (5). But would these outcomes differ from other manual therapies or exercise?
Another study demonstrated that lumbar mobilizations can immediately increase SLR range of motion compared to static stretching (6). What can we infer from this? Not much that’s directly relevant to HSI rehab unfortunately . However, there’s no harm in having a look at the lumbar spine, or going on to mobilize, manipulate, slide or tension the nervous system. Just go back and re-test your asterisk sign, and then contextualize changes within a positive message that affirms your patient’s health and self efficacy. And don’t fall in love with these short term changes. Move it, re-test, and move on!
As with most things in manual therapy, we can temporarily improve pain and function, which does have a role early in the rehabilitation process; but, the progressive hamstring, trunk stability, and proprioceptive exercises are the clear winners as they are interventions proven to enhance recovery, minimize recurrence, and provide a protective effect against future HSI. Not only does exercise provide long-lasting physiological changes to the issue in the tissue, it increases patient self-efficacy. If our patients know how to manage their condition and understand how to prevent it, we increase the probability of a favorable prognosis.
- Get patients moving quickly. Achieve Goldilocks Activation using irritability as a guide. Go on to progressively advance an exercise program that targets the trunk, hamstrings and any other impairments found on examination.
- Shape Expectations: relay positive messages of a favorable prognosis and the importance of a maintenance program for those returning to sport early.
- Be an effective pain-modulator: use manual therapy directed at the lumbar spine (i.e. manipulation, mobilization, or neurodynamics) or to other lower extremity joints and structures to reduce pain and increase function.
SEAN OVERIN, BHK, MPT
BRADLEY JAWL, BSC, MPT
References:- Sherry, M. Best, T. A Comparison of 2 Rehabilitation Programs in the Treatment of Acute Hamstring Strains. JOSPT. 2004.
- Gabbe BJ, Bennell KL, Finch CF, et al. Predictors of hamstring injury at the elite level of Australian football. Scand J Med Sci Sports 2006.
- Henderson G, Barnes CA, Portas MD. Factors associated with increased propensity for hamstring injury in English Premier League soccer players. J Sci Med Sport 2010.
- Heiderscheit, B. Sherry, M. Silder, A. Chumanoz, E. Thelen, D. Hamstring Injuries: Recommendations for Diagnosis, Rehabilitation, and Injury Prevention. JOSPT. 2010
- Yolanda Castellote-Caballero, Maríe C. Valenza, Emilio J. Puentedura, César Fernández-de-las-Peñas, and Francisco Alburquerque-Sendín. Immediate Effects of Neurodynamic Sliding versus Muscle Stretching on Hamstring Flexibility in Subjects with Short Hamstring Syndrome. Journal of Sports Medicine. 2014.
- Szlezak, A. Georgilopoulos, P. Bullock-Saxton, J. Steele, M. The immediate effect of unilateral lumbar z-joint mobilization on posterior chain neurodynamics: a randomized controlled study. Manual Therapy. 2011.