I recently spoke with a few students, new grads, and experienced clinicians about pain science verses biomechanics. Often people are seeing this as an either or decision! In fact, on a few occasions I have heard new grads and students say, “I want to be exposed to both and then I will decide which way to practice.” This blog is targeted at those struggling to find their way in this area, and to discuss how we might integrate both concepts into our practice without being blind to the other (much thanks to Greg Lehman for all his work and influence in this area).
I am obviously biased in this area, so I will admit up front that my bias is to pain science clinical reasoning. But it is important to take stock of where biomechanics may or may not apply.
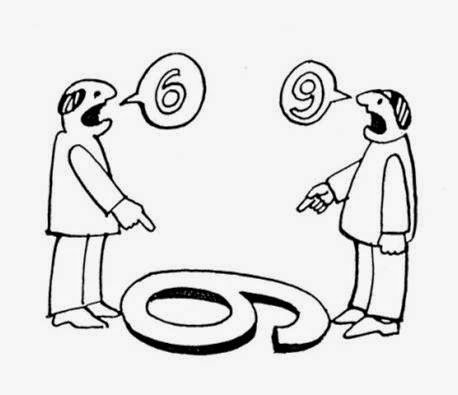
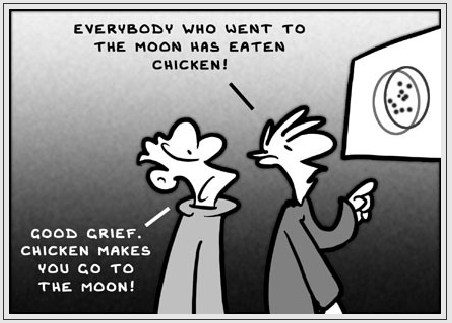
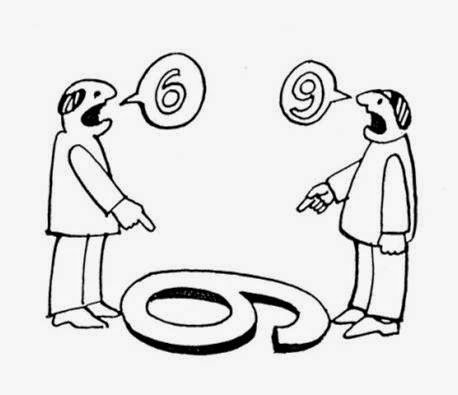
Be careful with your biases. Your perspective does not equal reality.
Let’s define our terms & then talk about a few areas of contention:
Biomechanics: the study of how the systems and structures of biological organisms, from the smallest plants to the largest animals, react to various forces and external stimuli. In humans, biomechanics often refers to the study of how the skeletal and musculature systems work under different conditions. In biomechanics more generally, scientists often try to apply physics and other mathematically based forms of analysis to discover the limits and capabilities of biological systems (
Ref).
Pain science: here is the definition of pain neuroscience education (PNE):
Instead of a traditional model of connecting tissue injury or nociception and pain, [PNE] aims to describe how the nervous system, through peripheral nerve sensitization, central sensitization, synaptic activity, and brain processing, interprets information from the tissues and that neural activation, as either upregulation or downregulation, has the ability to modulate the pain experience. Patients are thus educated that the nervous system’s processing of their injury, in conjunction with various psychosocial aspects, determines their pain experience and that pain is not always a true representation of the status of the tissues. By re-conceptualizing their pain as the nervous system’s interpretation of the threat of the injury, rather than an accurate measure of the degree of injury in their tissues, patients may be more inclined to move, exercise, and push into some discomfort. (
ref: Louw et al., 2011)
As such, for our purposes we will infer that Pain Science (as a clinical reasoning framework) could be defined as:
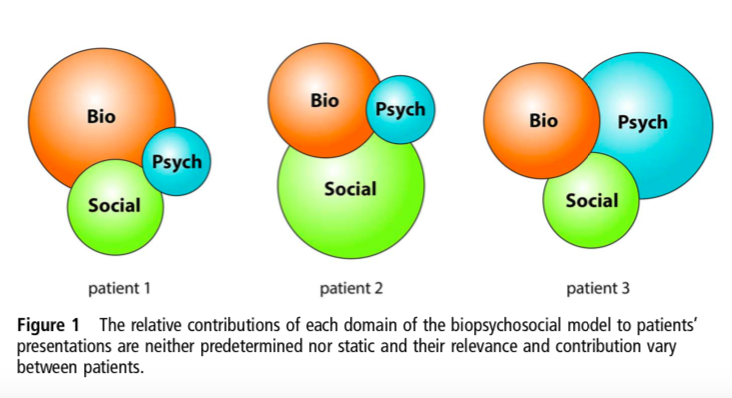
The understanding is that pain is an output of multiple inputs that are processed by the central nervous system based on all the organism’s past experiences, biases, and assumptions. This output (pain) is designed to protect the organism. The inputs can be biological, psychological, or social in nature (i.e. a biopsychosocial model of pain).
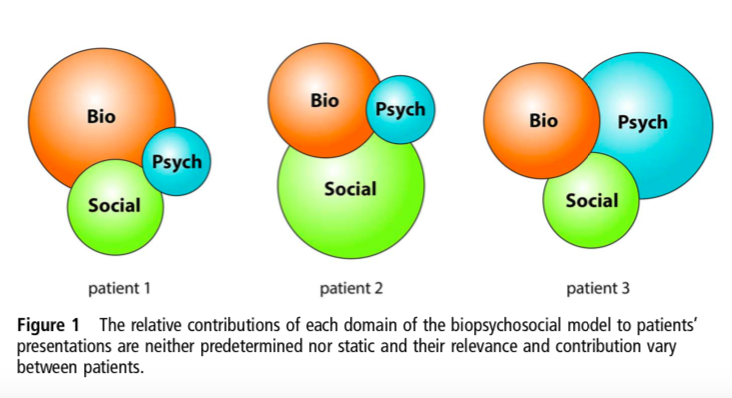
Gwen Jull represents the variety of influence from the different domains of the biopsychosocial. Meet your patient were they are at!
We can already start to see that biomechanics could have a role in understanding the biological input to the nervous system and that pain neuroscience, as understood from a biopsychosocial (BPS) framework, can include the effects of biomechanics on the protective system of pain. Unfortunately, in the world of MSK healthcare, a divide has grown between therapists that were trained and subscribe to biomechanical/biomedical reasoning and the growing world of pain science. The battlefront is often seen on social media platforms, and often doesn’t seem to resolve in mutual understanding, but rather escalates and entrenches the participants in their own beliefs (see an earlier blog on the backfire effect
here).
So let’s take a look at a few areas of contention in this debate in the hopes of discovering how we can bridge this clinical divide.
It depends… Acute tissue damage may require altering loads for a short period to gain control over symptoms and healing. However, this is the function of pain in this case, and where biomechanics can help us understand how to attenuate tissue loading. There is clear evidence that biomechanical principles help us understand that acute increases in loads put our tissues at risk of injury. This happens both in an instant, as with ACL ruptures (lateral trunk & knee abduction moments (Ref), flatfooted or hind-footed ground contact, knee abduction and increased hip flexion may be risk factors for ACL injury (Ref)), as well as over bouts of training (acute:chronic work load (Ref, ref, ref), which support the biomechanical principles of arthrokinematics, osteokinematics, load managements, and adaptation contribution to pain and injury. In these cases loads exceed capacity of the tissues resilience resulting in damage to tissue.
However, these conditions are neither necessary or sufficient circumstances to explain the experience of pain (
Ref). As an example, in 1995 Fisher and colleagues published an emergency department case in which a 29 year-old builder had stepped on a 15 cm nail. As he was in significant pain, with the slightest movement of the nail causing agony, he was sedated and the nail was removed (
Ref). However, upon inspection the foot was entirely uninjured, as the nail had gone between his toes despite being proximal to the steel toe of his boot. This is an example of tissue damage not being necessary for pain.
When signs of tissue damage are not painfully obvious (pun intended) then altering load on biomechanics principles leads to a slippery slope of reasoning. However, this is to say that pain science and respecting symptom irritability do go hand-in-hand. The concept of monitoring irritability goes back a long way in many clinical reasoning methodologies (Maitland, McKenzie, Mulligan, etc.), however, pain science allows us to say it is ok if a patient experiences pain, and that avoiding pain altogether is not necessary for good outcomes nor is it a helpful message to send to patients that pain is always in charge. In fact, a systematic review and meta-analysis by Smith (2017; Ref) examining the role of painful versus pain-free exercise in the management of persistent musculoskeletal pain (>3 months) concluded that protocols involving painful exercises demonstrated significant short-term improvements over pain-free exercise; however, this difference was not seen maintained over the medium or long term.
Yes! And… (“Yes, and” is basically the theme of this blog – Thanks Jeff Moore) Frequently reassure patients that it is safe to move/pace-up despite their symptoms.
Obviously moving well and understanding how to move objects well is important to performance, that is why sports biomechanics is a field. A study by Weinchester (et al., 2005; Ref) demonstrated that 4 weeks of 3 times weekly technique coaching improved the performance of the power clean Olympic lift in those with at least one year experience with this movement (basically picking a heavy barbell off the floor up to your shoulders). They observed that with technique focused training subjects improved both power, force, and velocity of the bar, as well as improved bar path (roughly less horizontal movement of the bar leading to the bar getting higher off the ground with a straighter path).
Similarly, leg stiffness (i.e. minimal change in leg length with high ground reaction force) is associated with improved sprint performance, and the movement and coordination is an important aspect of coaching sprint athletes (Harrison 2010; Ref). A study of competitive Olympic weightlifters showed that initial direction of bar velocity predicted success verses unsuccessful snatch lifts (again lifting a heavy bar off the ground, but this time over head) (Gourgouils et al., 2009; Ref). Interestingly, there were no other differences in kinematics or kinetics of the lower limb and bar that predicted success.
These studies suggest skilled movement can be taught, learned and improve performance. However, the story doesn’t stop here. Performance is influenced by psychosocial variables as well (this is why there are sport psychologists). Gould and colleagues (1999; Ref) identified that for successful Olympic team sports experienced, “crowd and family or friend support, utilized mental preparation, and were highly focused and committed. Teams that failed to meet expectations experienced planning and team cohesion problems, lacked experience, faced travel problems, experienced coaching problems, and encountered problems related to focus and commitment.”
A very interesting study by Moore (et al., 2012; Ref) examined the effects of “challenge” or “threat” states on performance of a golf putting task. Briefly, these authors explain that prior to a task the individual evaluates whether they have the resources to cope with the task demands. If they evaluate that they have the resources, then a challenge state arises (associated with positive and negative emotions, improved performance and increased cardiovascular function), if not then a threat state arises (associated with negative emotions, poor performance, and decreased cardiac function).
Moore and colleagues found that by manipulating the task instructions and setting positive or negative expectations for the golf putting task, threat state participants demonstrated lower performance (further from the hole), which was mediated by changes in swing kinematics and resultant movement quality. Additionally, threat states were also associated with higher cognitive anxiety states. (Does this sound familiar to another neuro-regulated system… one designed to protect the organism?) So, moving well and efficiently can affect performance, but psychological and social factors can influence it as well. Thus, in the arena of performance, even without considering pains impact on performance, it is an “and” not “or” conversation.
"Moving well and efficiently can affect performance, but psychological and social factors can influence it as well."
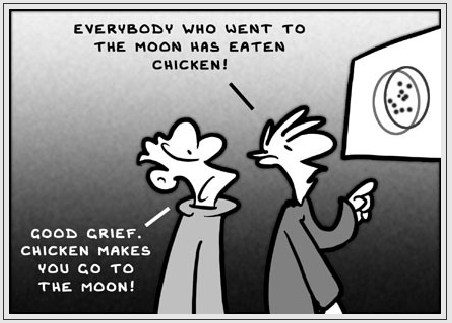
This is where I think the huge disagreement exists. There is huge debate on how manual therapy works, and thus how physiotherapists view hands-on therapy, assessment, and clinical reasoning (notice the order here). The big issue in my mind is that we have to be careful not to commit an ad hoc, ergo propter hoc logical fallacy (i.e. I reason this, after this reasoning a positive result followed, thus my reasoning was correct). We must admit that when it comes to how manual therapy works (which for pain modification, it seems to work well) we are dealing with very large uncertainty (Thanks to Brad Jawl and his great for the next part).
“Traditionally joint targeted manual therapy has been based on a detailed biomechanical assessment of the motion segment (i.e. the joint) where the lack of normal osteokinematics is noted, and becomes the target of intervention to restore “normal” function. This reasoning makes the assumption that it is first possible to detect a lack of normal osteokinematics with such assessment techniques, and then that specific manual therapy moves the motion segment to correct such a “dysfunction.” Let’s examine these assumptions:
- Can we accurately detect alterations in motion at a motion segment?Here we will discuss spinal motion palpation simply because it has been the most widely studied. A literature review on the reliability of spinal motion palpation concluded (Ref):
- Intrarater agreement varies from less than chance to generally moderate or substantial agreement.
- Interrater agreement only rarely exceeds poor to fair agreement.
- Rating scales measuring absence versus presence or magnitude of pain response yield higher agreement values than mobility rating scales.
- Can we manually mobilize or manipulate a motion segment in the specific direction?
- In this case we can ask if manual therapy is specific, or if we can move a motion segment in a specific direction? The research in this area shows us that we are neither specific to a segment (cavitation occurred at least one vertebra away from the target of lumbar manipulation 54% of the time; Ref) nor able to move that segment in a specific direction (only forces perpendicular to the skin surface contribute to movement due to a near frictionless skin fascia interface Ref, ref).
Without attempting to answer why it works, it is important to note that there is mounting evidence that says manual therapy does work. Multiple studies have found that there is no difference in the short-term analgesic effects of spinal manual therapy when directed at a therapist determined or randomly selected segment of the cervical and lumbar spine (Ref, ref)
Additionally, a 2009 review of the literature on manual therapy in the treatment of pain (Ref) suggested the mechanism likely is exerted by some combination of the effects on the local tissue, peripheral, and central nervous system via neurophysiological affects.”
However, rather than assuming that this means we must walk away from manual therapy all together, it should more importantly open options on how we use it clinically, and maybe more importantly, how we explain it to patients. Again, if we reason that we must intervene with manual therapy due to a biomechanical finding, we apply manual therapy and it works, our human nature for conformation bias will strengthen our belief that our logic was correct. And one of the largest reason that this is an issue, is because when we believe the biomechanical system is at fault, we will explain it that way to patients. And we know that biomechanical and biomedical explanations for pain can foster feelings of fragility for our patients (see examples below). Shouldn’t we instead be focusing on the capacity and adaptability of the human body to send a message of hope!
Lots more to cover so look for part 2 of this blog next week!