Mar 28
/
Hélène Thériault, BScOT, MAdEd, MCC
Beyond Advice-Giving: Why Healthcare Needs a Coaching Revolution
As an occupational therapist with over a decade of experience, I was always searching for ways to help my clients create meaningful, lasting change. But no matter what strategies I tried, I kept running into the same frustrating pattern: patients weren’t following through.
I could prescribe the best interventions, provide all the education, and outline the clearest plan—but something wasn’t clicking. My clients weren’t following through and I was starting to feel the weight of it. I was working harder than they were, desperately wanting to support them. Over time, I wasn’t just exhausted; I was wondering how sustainable working in healthcare was for me. That’s when I discovered coaching.
Rethinking Patient Care: The Role of Coaching in Healthcare
I signed up for a coaching workshop when I took on a new clinical leadership role. This new responsibility was taken on alongside my clinical work, and I wanted to expand my ability to support my team.
The course wasn’t designed for healthcare providers: it focused on workplace settings rather than clinical interactions. However, with years of studying adult education theories, especially the transformative learning theory, which focuses on how deep, lasting change occurs through shifting perspectives—I saw a clear connection. The core principles of coaching aligned with what I already knew about how people learn and grow.
That’s why I sat there, mouth agape—Could this be applied in healthcare? Was this the missing piece in healthcare—one that could help clients achieve their rehabilitation goals while also preventing my own burnout?
I later discovered the answer was a resounding YES.
I had to trust the theory—and I chose to do so through experimentation. I started applying coaching techniques with my most challenging patients—ones who had been stuck for months, recovering from concussion, PTSD, and severe depression. Instead of telling them what to do, I asked different kinds of questions. I listened differently—I gave them space to reflect, rather than rushing in with solutions. After a while, I noticed a shift. For the first time, they moved forward—not because I pushed them, but because they took ownership of their progress.
That was the moment I knew that coaching wasn’t just for leadership. It had a place in healthcare. However, at the time, I wasn’t aware of any training or framework designed by or for healthcare professionals on how to apply coaching principles with patients and clients.
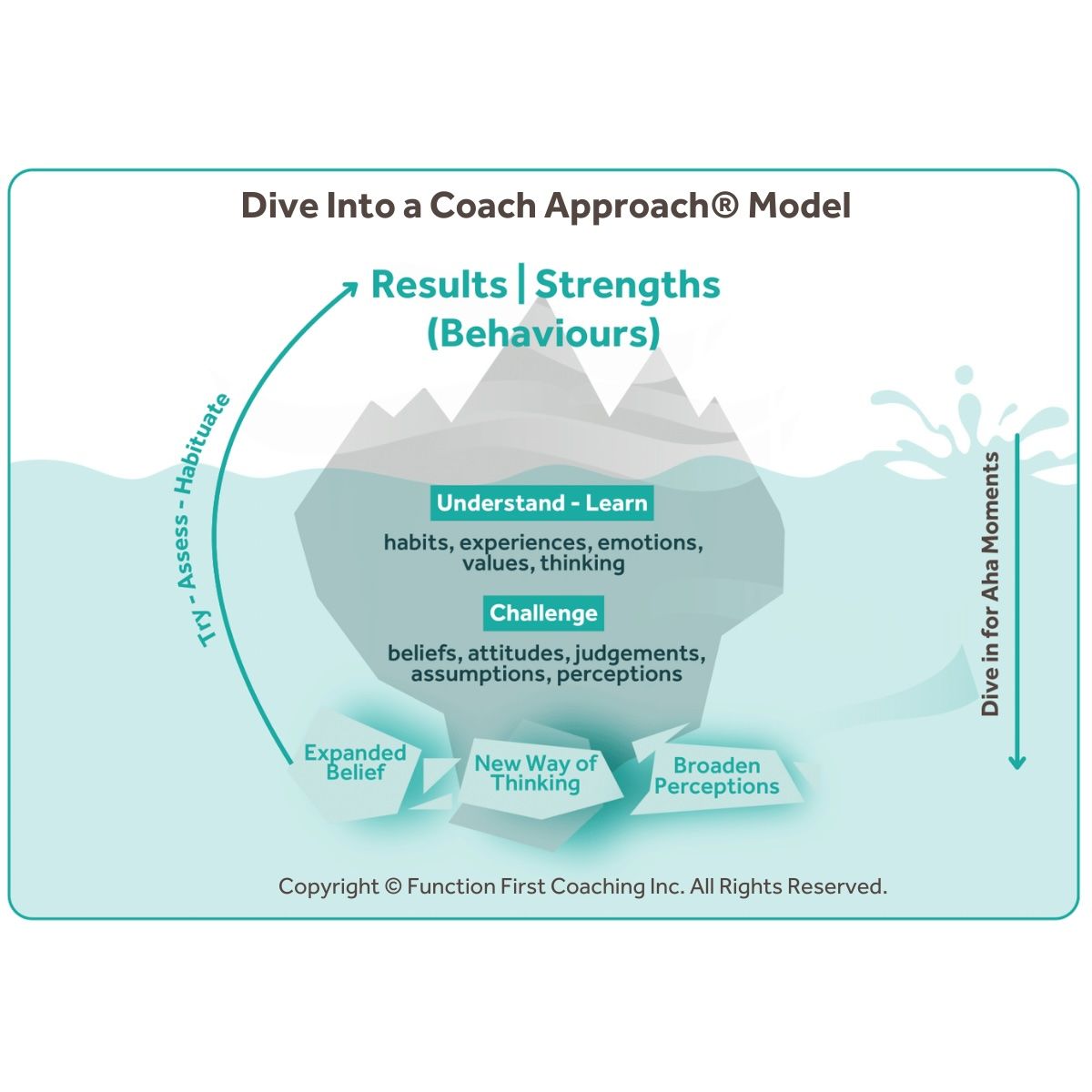
That’s why I developed Dive Into a Coach Approach®—a model specifically designed to help healthcare professionals integrate coaching into their patient care. Today, it includes a 50-hour accredited certification program and has established a clear definition of coaching in healthcare:
A semi-structured conversational partnership where concrete action plans are co-developed through accessing individuals’ strengths, resources, and creativity with the intent to: a) empower clients to get their occupational wants or needs met; b) enable sustained change through meaningful self-directed actions. (Hélène Thériault, 2025).
Why Traditional Advice-Giving Falls Short in Healthcare
- Patients often already know what they should do—they just struggle to do it. A systematic review found that medication non-adherence among patients with multimorbidity is widespread, with a pooled prevalence of 42.6% (Foley et al., 2021), highlighting the need for approaches beyond advice-giving.
- Information alone doesn’t lead to transformation—internal motivation does. Research indicates that intrinsic motivation, driven by personal satisfaction, is often more sustainable and leads to longer-lasting behavior change.
- The expert-driven model creates a one-way flow of advice, rather than a partnership. Shifting to a partnership model, where patients are actively involved in their care, has been shown to improve health outcomes and patient satisfaction.
How Coaching Transforms Patient Engagement and Outcomes
Tamara Shih, a Physical Therapist in California, discovered that a Coach Approach can completely change the way patients engage with treatment.
Many healthcare professionals have experienced the pressure of being the expert who has all the answers. However, shifting from a fixer role to a facilitator role can be transformational—for both the provider and the patient.
Instead of prescribing rigid solutions, she partnered with patients to co-develop strategies that worked for them.
"When I first started learning about the Coach Approach, I started playing with it immediately because it seemed like such a great way to really get to the bottom of why patients weren’t adhering to their home exercise programs or why they weren’t getting to the goals they wanted to reach.”
Rather than simply telling patients what to do, she began coaching them to uncover their own solutions. And the results were profound.
"I've just gotten feedback from patients that the physical therapy they get with me is different from any other physiotherapist they’ve had before. They say, ‘You actually hear me. You listen to me. I understand why I have to do these exercises, so I do them.”
Many healthcare professionals have experienced the pressure of being the expert who has all the answers. However, shifting from a fixer role to a facilitator role can be transformational—for both the provider and the patient.
A Physiotherapist in Ontario Canada, Susan Czyzo, described how this shift lightened her mental load while improving patient outcomes:
"Moving out of that 'fixer' role took so much pressure off me. Instead of constantly thinking, ‘What solution am I going to provide? What advice can I give?’ I now have space to actively listen. And that leads to more meaningful sessions and stronger connections with my clients, which I truly value—and I know they do too."
But it’s not just about reducing stress for providers—it’s about activating patients in their own recovery process. Tamara shares how this shift fundamentally changed how she approached treatment plans:
“I was working too hard for my patients—constantly trying to figure out when they could fit exercises into their routine. Now, instead of me doing all the problem-solving, I ask them: ‘When do you think this could be integrated into your daily routine?’”
Instead of prescribing rigid solutions, she partnered with patients to co-develop strategies that worked for them.
"I’ve had patients come back and say, ‘Oh, I figured out I can do it at this time, and it’s doable!’ That’s exactly what I want—for them to take ownership of their recovery.”
Real-World Applications of Coaching in Healthcare
On the surface, coaching might seem as simple as asking good questions. But as Miller et al. (2018) observed, one of the most foundational coaching competencies—active listening—is also one of the hardest to master. Research on doctor-patient communication confirms this—patients report higher satisfaction and better adherence when they feel truly heard (Gu et al., 2020; Hashim, 2021).
"Coaching seems simple—until you try it."
Why a Coach Approach Works in Healthcare
A Coach Approach shifts healthcare professionals from fixers to facilitators—helping patients tap into their own motivations, values, and solutions.
As Tamara puts it:
✔ Patients become active participants—leading them to better follow-through and adherence.
✔ It supports behavior change more effectively—moving from short-term compliance to long-term lifestyle shifts.
✔ Stronger therapeutic relationships—patients feel heard, valued, and engaged.
✔ Less burnout for providers—because the responsibility for change is shared rather than falling entirely on the clinician.
As Tamara puts it:
“I was getting really burnt out trying to do everything for my patients. Now, adding a Coach Approach to what I am already doing as a physical therapist, they take on some of that responsibility—because it’s their body, and they need to own that partnership in their care.”
The Future of Healthcare is Collaborative:Shifting from Advice-Giving to a Coach Approach
If you’re a healthcare professional, you don’t have to overhaul your practice overnight. You can start small:
✅ Ask more, tell less: Instead of leading with advice, lead with questions.
✅ Partner on solutions: Work with patients to create realistic plans that fit their lives.
✅ Embrace silence: Patients often need time to process and reflect—don’t rush to fill the gap.
What a Coach Approach Can Do For You
Healthcare is changing. Patients want more than just information, they want to be engaged, heard, and empowered. A Coach Approach isn’t just a technique—it’s a mindset that:
✔ Creates better patient outcomes
✔ Reduces clinician frustration
✔ Strengthens healthcare relationships
I never expected coaching to change the way I saw healthcare. But once I did, I knew I could never go back.
What's Next?
If this resonates with you, take a moment to reflect:
💡 How do you currently engage your patients?
💡 What would change if you shifted from advice-giving to coaching?
A small shift in how we communicate can make a world of difference—for both patients and healthcare professionals alike.

Ready to Dive in?
Join Hélène Thériault for Dive Into A Coach Approach®!
Hélène Thériault, BScOT, MAdEd, MCC
References
- Alcorn, K., & Broome, K. (2014). Occupational performance coaching for chronic conditions: A review of literature. New Zealand Journal of Occupational Therapy, 61(2), 49-56.
- Barr, J. & Dowding, L. (2022). Communication in Leadership. In Leadership in Healthcare- 5th Edition. Sage Publication.
- Cook, E., Greene, G. J., & Maxwell, J. (2024). Coaching for person-centred healthcare: A solution-focused approach to collaborative care (1st ed.). Taylor & Francis Group. https://doi.org/10.4324/9781003414490
- Dejongue, L.A., Becker, J., Froboese, I., Schaller, A. (2017). Long-term effectiveness of health coaching in rehabilitation and prevention: A systematic review. Patient Education and counselling, 100, 1443-1653.
- Elster, M. O’Sullivan, P.S., Muller-Juge V., Sheu L., Kaiser S.V., Hauer K.E. ( 2022). Does being a coach benefit clinician-educators? A mixed methods study of faculty self-efficacy, job satisfaction and burnout. Perspect Med Educ. 11(1):45-52. doi: 10.1007/s40037-021-00676-7.
- Foley, L., Larkin, J., Lombard-Vance, R., Murphy, A. W., Hynes, L., Galvin, E., & Molloy, G. J. (2021). Prevalence and predictors of medication non-adherence among people living with multimorbidity: A systematic review and meta-analysis. BMJ Open, 11(9), e044987. https://doi.org/10.1136/bmjopen-2020-044987
- Graham, F., Kennedy-Behr, A., & Ziviani, J. (2021). Occupational performance coaching: A manual for practitioners and researchers. New York, NY: Routledge.
- Gu, A., Yue, Y., Wang, Y., Guo, L., & Yu, Y. (2020). Physician-patient communication and self-care behavior in patients with hypertension: A cross-sectional study. BMC Health Services Research, 20(1), 1-9. https://doi.org/10.1186/s12913-020-05912-0
- Haynes, A., Sherrington, C., Ramsay, E., Kirkham, C., Manning, S., Wallbank, G. (2022). Sharing success with someone: Building therapeutic alliance in physiotherapy-delivered physical activity coaching for healthy aging. Physiotherapy Theory and Practice. 23 (13).
- Hashim, M. J. (2021). Patient-centered communication: Basic skills. American Family Physician, 103(12), 757-762. Retrieved from https://www.aafp.org/pubs/afp/issues/2021/0615/p757.html
- Lin, S., Dongzia, X., Chamberlain, D., Newman, P., Xie S., Tan, J.-Y. (2020). The effect of transition care interventions incorporating health coaching strategies for stroke survivors: A systematic review and meta-analysis. Patient Education and Counseling, 103 (10), 2039-2060
- Mair, J. L., Salamanca-Sanabria, A., Augsburger, M., Frese, B. F., Abend, S., Jakob, R., Kowatsch, T., & Haug, S. (2023). Effective behavior change techniques in digital health interventions for the prevention or management of noncommunicable diseases: An umbrella review. Annals of Behavioral Medicine, 57(10), 817-835. https://doi.org/10.1093/abm/kaad041
- Ogourtsova, T., O'Donnell, M., De Souza Silva, W., & Majnemer, A. (2019). Health coaching for parents of children with developmental disabilities: A systematic review. Developmental Medicine and Child Neurology, 61(11), 1259-1265. https://doi.org/10.1111/dmcn.14206
- Pentland, W., Isaacs-Young, J., Gash, J., & Heinz, A. (2016). Enabling positive change: Coaching conversations in occupational therapy. Ottawa, ON: CAOT. Publications ACE.
- Salazar II, R. (2022). Better outcomes: A guide to humanizing healthcare. Business Expert Press, LLC. New York, NY.
Subscribe to our newsletter
Every Friday we cover must read studies, how they fit in practice, give it real world context, provide top resources and one sticky idea.
Thank you!
You have successfully joined our Friday 5 Newsletter subscriber list.
